Accessing the pterygoid area and successfully placing implants might be seen as a challenging case for implantologists since the posterior maxilla has different limitations in the form of bone quality, quantity, anatomy of the maxillary sinus and accessibility. Placement of implants into the pterygoid-maxillary region opens new ways in the rehabilitation of the atrophic posterior maxilla.
ROOTT P
The special characteristics of the ROOTT P implant such as:
- Self-drilling;
- Self-tapping;
- Self-condensing;
- Thin apex, wide threads;
- Strong and secure screw.
The pterygoid implant was introduced to solve the problem of implant restoration in the posterior maxilla due to the presence of the sinus and also as a result of the limited bone quality of bone in this region.
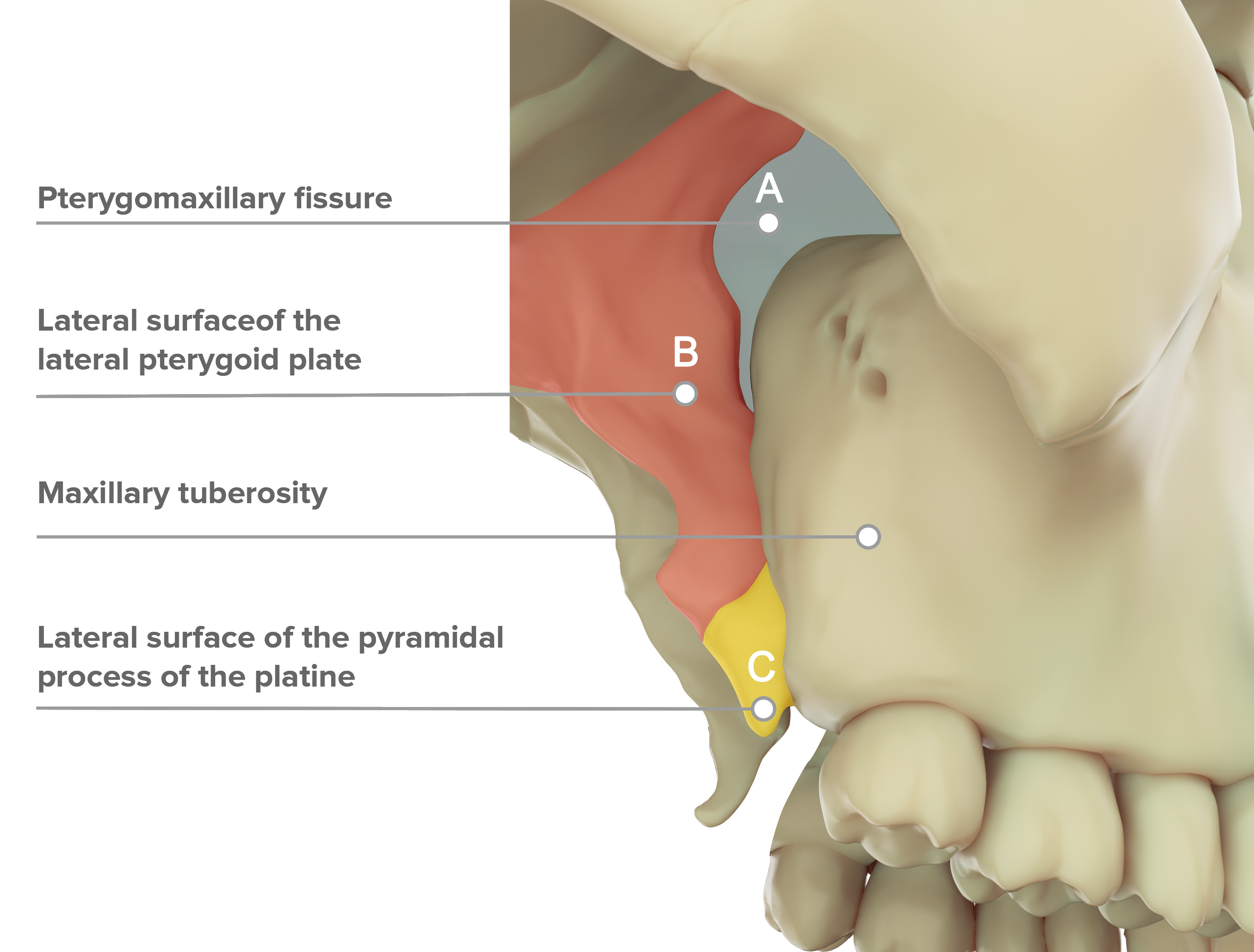
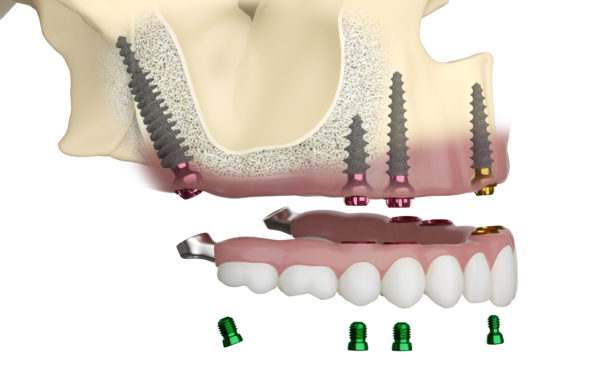
The ROOTT P implant is anatomy adapted implant, it features a thin self-tapping apical thread that engages easily in the cortical pterygoid process and a bold implant body with thick large threads specifically designed to condense the trabecular bone present in the maxillary tuberosity (Fig. 1)
The implant neck features a broad thread profile that offers compression in the tuberosity area, where bone density is frequently limited. The pterygoid implant’s length guarantees and engages the implant apex in the cortical bone of the medial wall of the pterygoid plate, resulting in maximal cancellous bone compression by the implant’s immense threads.
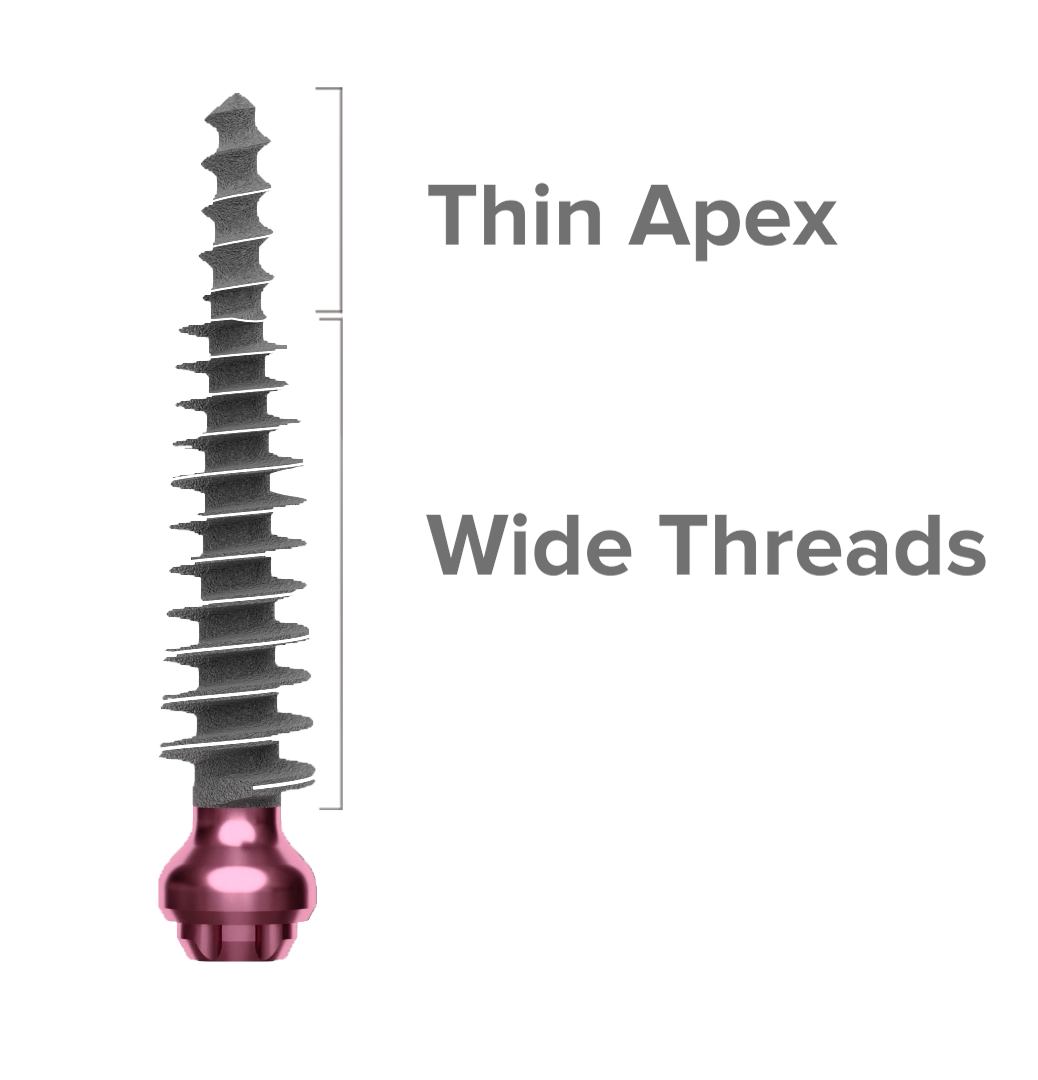
Fig. 1
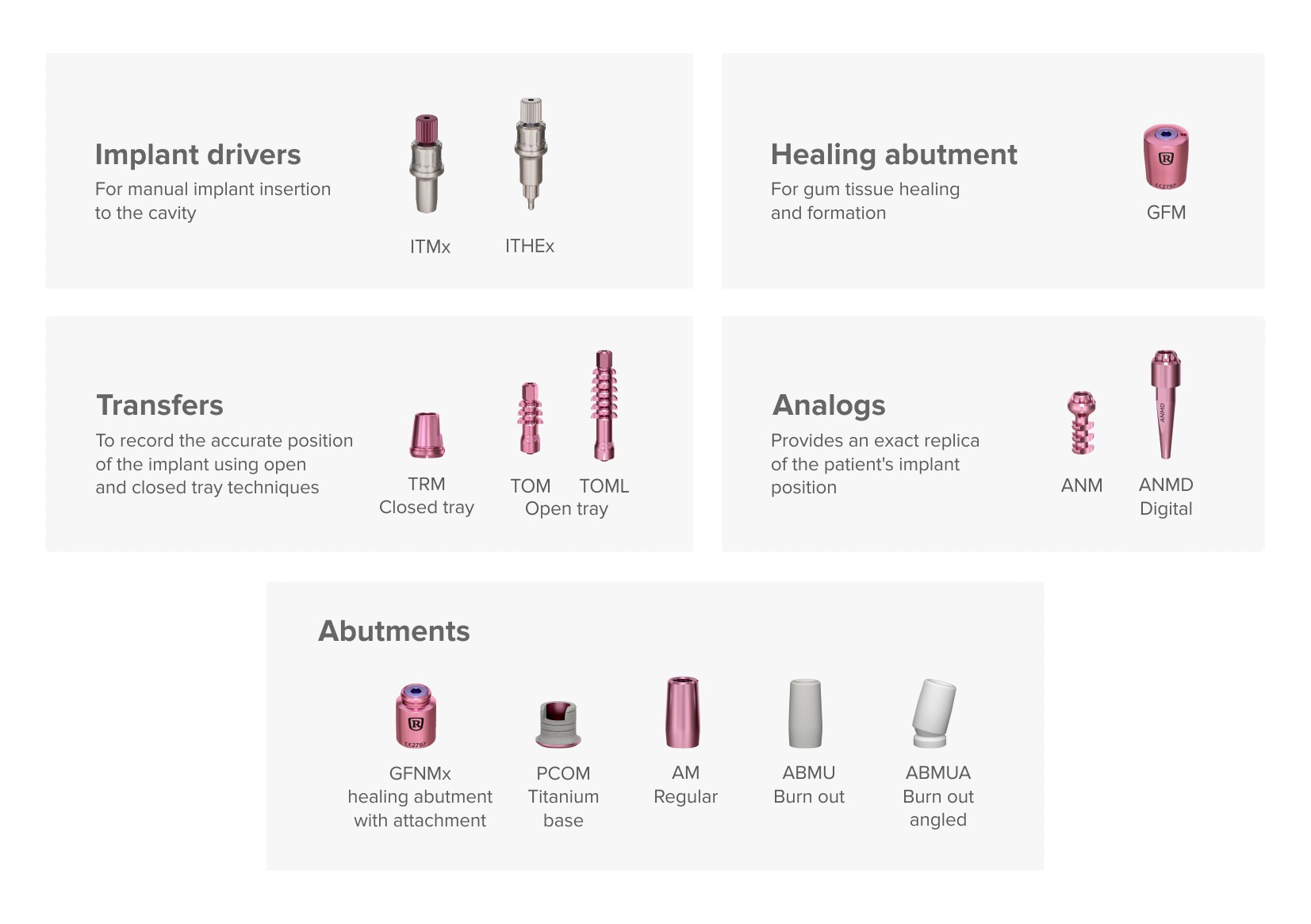
For the Pterygoid implants, a different insertion technique is used. This can be manual insertion without drilling. For the surgical technique, a single drill is used at a working speed of 600 rpm and the implant insertion is done by hand (manually). This technique is termed the Soft technique.
Axial and non-axial force resistance after osseointegration with ROOTT P can be established.
Fig. 2
Avoids complications
Alternatives such as zygomatic implants for posterior maxilla rehabilitation can often cause additional complications. Tearing the sinus membrane during sinus lifting procedures, seepage of grafts into the sinus. Furthermore, the loss of bone grafts due to bone resorption after bone augmentation procedures. Higher chance of consequences and complications after zygomatic implants. Such complications as: oroantral fistula formation, orbital penetration and injury, temporary sensory nerve deficits and vestibular cortical fenestration (F. Tzerbos et. al. 2016).
If we take a look and compare the process of zygomatic implant and pterygoid implant placement, we can notice the invasiveness difference between implanting procedures.
- tear of the sinus membrane during sinus lift procedures, seepage of bone grafts into the sinus,
- loss of bone grafts due to bone resorption after bone augmentation procedures,
- high morbidity.
Controlling pterygoid region with ROOTT P
Taking into consideration that the pterygoid region has a significant amount of anatomical obstacles, not many specialists are considering pterygoid implants and going for more familiar options such as zygomatic implants.
Safer, less invasive option for patients and specialists. Implants placed in the pterygomaxillary area are angulated without the application of direct axial pressures to the implant. Nevertheless, once osseointegrated, reports (Agbaje JO, H. Diederich, 2018) show that these implants withstand all axial and non-axial pressures better than any other maxillary implant. Furthermore, the patient tolerates the implant well, without any complications with speech or oral hygiene maintenance. The rehabilitation of the posterior maxilla with pterygoid implants is advantageous because the implants are biomechanically stable and have cantilever pontic.
Because the anatomy of the pterygomaxillary region varies greatly across individuals, a customized pre-surgical radiologic examination should be done whenever a pterygoid implant is intended to be put in this location. Several variables influence bone density in the pterygomaxillary area, including dental status (edentulous patients have lower bone density), age (density declines with ageing), and gender (females have statistically lower bone density). Nonetheless, it has been demonstrated that the bone density of the pterygoid process is always greater than that of the maxillary tuberosity, and so it should be the preferred location for implant anchoring in an atrophic maxilla (Fig.2).
Avoiding bone augmentation and sinus lifting
Bone augmentation is often necessary to allow for the insertion of a sufficient quantity and length of implants to sustain the implant prosthesis. Insufficient bone for implant anchoring is frequently caused by low bone quality in the posterior maxilla, along with restricted vertical bone height due to sinus pneumatization and chronic periodontitis. Surgery is often used as a solution for periodontal gum disease, loss of teeth in the upper jaw and reabsorption of bone into the body after tooth extraction. Sinus lift surgery is especially difficult with prolonged healing of usually 6 months.
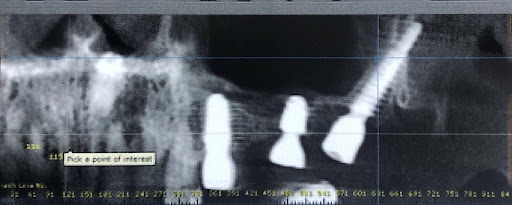
Fig. 4
Less invasive operations, time-saving options and patient-friendly rehabilitation can become aspects for which patients and specialists are looking. Due to angled insertion, thin apex and wide threads ROOTT P provides condensation in the region of the tuberosity, where the bone is often of low density.
ROOTT P compatibility:

If you want to hear more about ROOTT P implants, consider joining the Open Dental Community Congress 2022 on January 31st, Dubai, and visiting the ROOTT booth on AEEDC 2022 from February 1st — 3rd.
References
1. Tzerbos, F., Bountaniotis, F., Theologie-Lygidakis, N., Fakitsas, D., & Fakitsas, I. (2016). Complications of Zygomatic Implants: Our Clinical Experience with 4 Cases. Acta stomatologica Croatica, 50(3), 251–257. https://doi.org/10.15644/asc50/3/8
2. Agbaje JO, Diederich H. Minimal Invasive Concept for the Rehabilitation of Edentulous Jaw with One-piece Implants. Int J Case Rep Short Rev. 2018;4(2): 027-030